An update on the research project you've helped to fund
Childhood leukaemia:
Developing a new treatment to overcome drug resistance
We have supported Action Medical Research with grants totalling £30,000 for this study which is now in its final few months. This is exactly why we setup Team Lewis Trust. We couldn't save Lewis but our objective is to help other families by supporting research to improve cure rates.
December 2021
Background
Acute lymphoblastic leukaemia (ALL) is the most common cancer in children and young people with around 500 new cases diagnosed each year in the UK in people aged 19 years or younger. Almost a third of cases occur in children aged 4 years or younger. Between 70 and 100 of these children are diagnosed with a disease subtype called T-cell acute lymphoblastic leukaemia (T-ALL). It affects the lymphoid-cell-producing stem cells, in particular a type of white blood cell called T lymphocytes. Nowadays, most children diagnosed with T-ALL will be cured with intensive drug treatment. Sadly, in around 20 per cent, the cancer eventually comes back and is almost impossible to cure, as the leukaemia has become drug resistant.
The Project
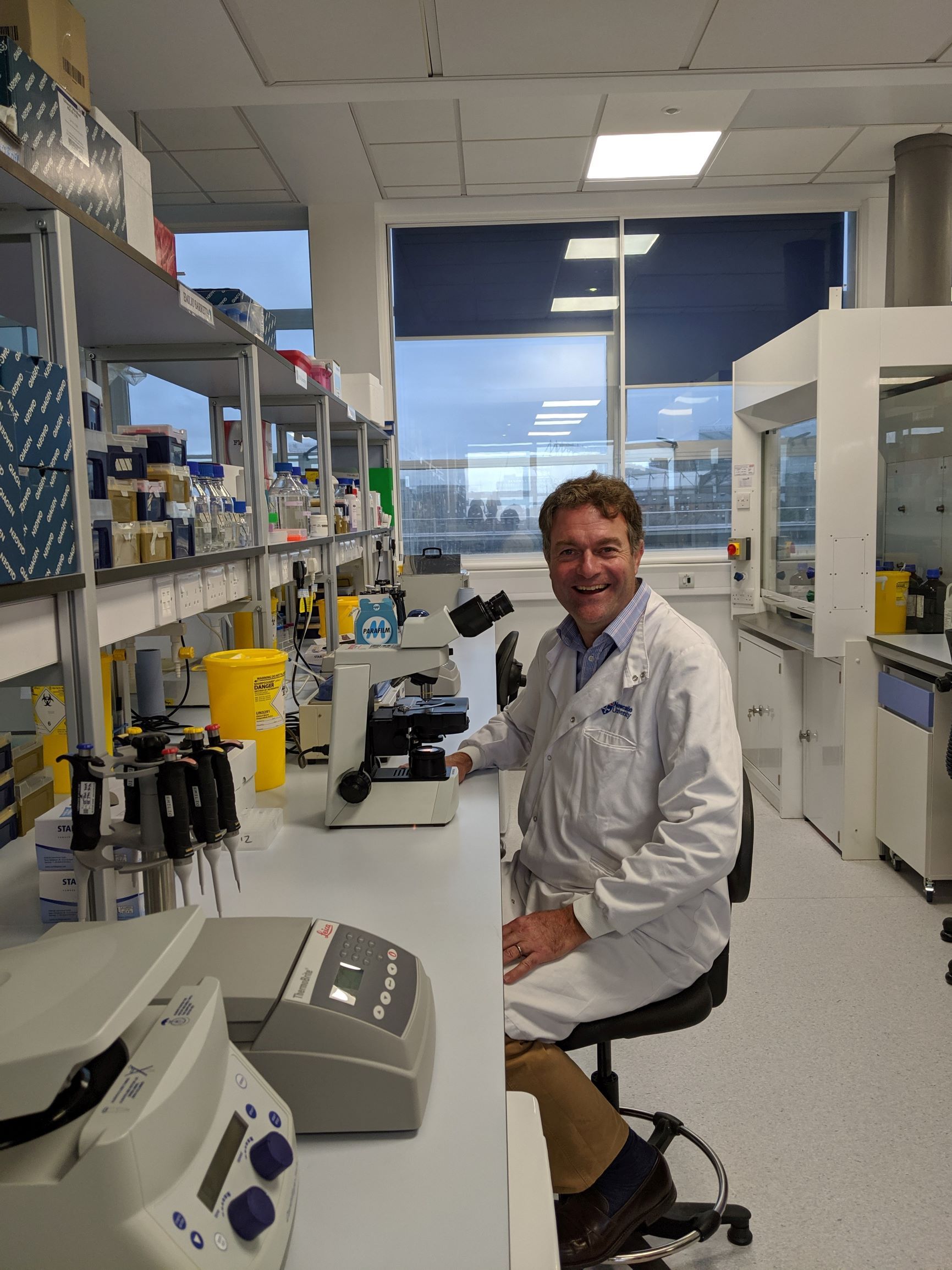
With the help of Team Lewis Trust, Action Medical Research has been supporting Dr van Delft and his team of researchers at Newcastle University and University of Glasgow. This three-year study aims to find out if combining two existing drugs could offer an effective new treatment option for children with T-ALL.
Glucocorticoid resistance is one of the main obstacles to achieving remission and a long-term cure for patients with recurrent or refractory T-ALL. Researchers had previously reported that the drug dasatinib (DAS), which blocks LCK – a signalling molecule identified as having a role in cell growth and proliferation – combined with dexamethasone (DEX), leads to decreased cell growth, as well as causing the death of leukaemia cells. The potential of DEX and DAS together (DEX+DAS), has been confirmed in a preclinical setting. As patients with T-ALL who no longer respond to steroids are unlikely to achieve remission, and qualify for a bone marrow transplantation, the new drug treatment combination, DEX+DAS, is an important finding. DEX+DAS has been included in a new international trial, designed to offer new treatments to patients with relapsed T-All, which will hopefully open in the UK in 2022.
While this drug combination is immediately clinically actionable, it is likely that combination with a third agent is required to achieve long term remission status in patients. The further aims of this project are the formulation of more potent drug combinations, identification of response biomarkers, and the study of the mechanism underlying the drug synergy between DAS and DEX.
Progress to date
Although COVID-19 restrictions have now been lifted, laboratory research was nevertheless limited throughout the pandemic. During lockdown the use of mice for drug testing was halted. However, the researchers overcame this hurdle and used their time well by developing a new drug testing system that will allow them to evaluate new drug combinations in patient cells. This is a very valuable system which supports the survival of patient cells long enough to perform studies and use an automated system to count the number of live and dead cells. The researchers are using this system to test specific blockers of proteins that usually keep leukaemia cells alive, and are testing these blockers on their own, as well as in combination with other drugs. The advantage of this system is that they can test multiple drug combinations in a petri dish, and only select the most promising drug combinations for studies in a mouse model, enabling a high throughput screening of drugs.
In the international trial next year, the use of DEX+DAS for patients with relapsed T-ALL will allow the researchers to see whether some patients achieve remission using this new drug combination, and ascertain whether any promising research results can be used to help patients in the future.
Work still to do
The remainder of this project will mainly focus on completing two specific aspects with the aim of publishing the findings in peer reviewed journals:
• Testing of triple drug combinations on patient derived cells in a petri dish to establish which patients might benefit from the addition of blockers of survival proteins. There is currently no publication that has assessed these drug combinations in T-ALL. As patient benefit is a priority, any promising results will be discussed with the trial steering committee.
• Validation of the biomarker test and integration of this test in the clinical laboratory setting to allow for accurate selection of patients who are likely benefit from DEX+DAS treatment.
Benefits to patients
This project has enabled the translation of a research idea, into a change in actual patient management:
‘To oversee laboratory studies resulting in new drug treatments for patients with a poor prognosis is very exciting. It allows a dream to become reality. This new drug treatment will be tried in actual patients with relapsed T-ALL in an international trial,’ Dr van Delft.
Dr van Delft will be responsible for the rollout of this trial in the UK to ensure patients here benefit from the new treatment approaches. Individual patient stories already suggest that this new drug combination will make a difference to the lives of families. It is expected that around 40 percent of patients with relapsed T-ALL may benefit from DEX+DAS treatment.
It is anticipated that this research could influence patient care in the next 2-3 years. The testing of triple drug combinations, and validation of a response biomarker for DEX+DAS, could lead to improvements in treatment of relapsed T-ALL.